Taking
LONSURF
HOW TO TAKE
LONSURF
Getting started on LONSURF treatment
Learn how to take LONSURF® (trifluridine and tipiracil) tablets
LONSURF® (trifluridine and tipiracil) tablets are:
- A tablet you swallow twice a day with food- the type of food does not matter
- A tablet you swallow whole
- Do not retake doses of LONSURF that are vomited or missed and continue with the next scheduled dose
LONSURF comes in 2 strengths: 15‑mg and 20‑mg tablets.*
Your healthcare provider may prescribe both strengths for your prescribed dose.
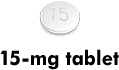 Actual tablet size is
Actual tablet size is 7 mm
for 15‑mg dose.
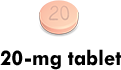 Actual tablet size is
Actual tablet size is 8 mm
for 20‑mg dose.
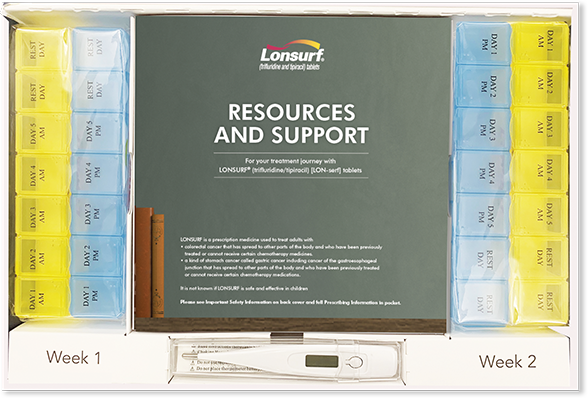
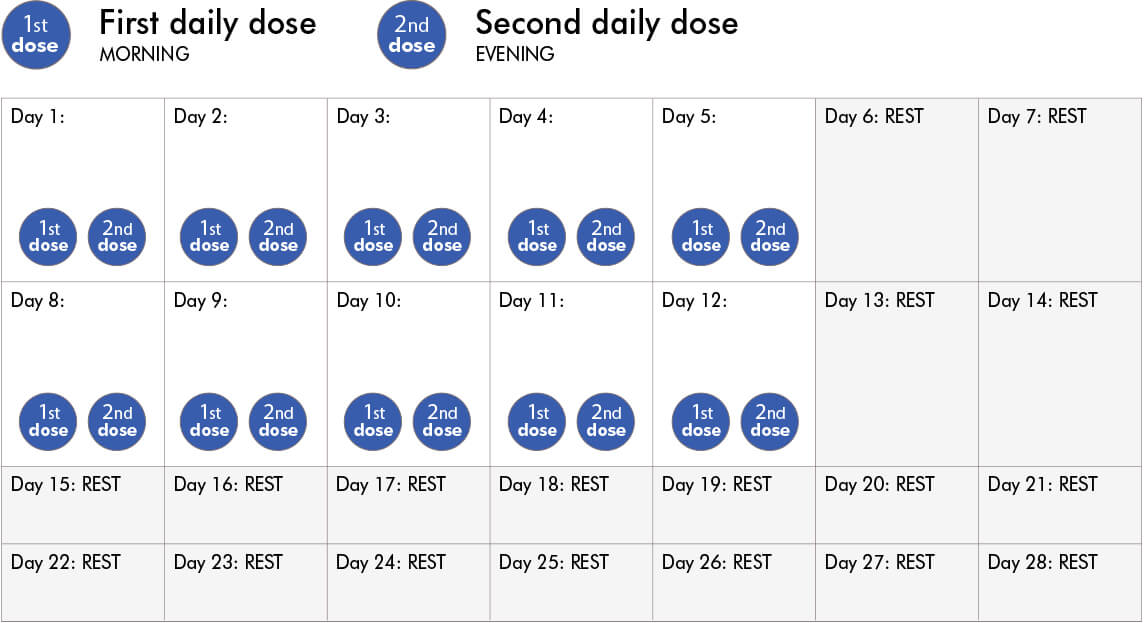
LONSURF 28‑day treatment schedule:
You will take LONSURF after morning and evening meals for 5 days a week, and then rest for 2 days. This goes on for 2 weeks.
Then you will not take LONSURF for 2 weeks (14 days).
This is repeated for as long as your healthcare provider says. Always follow all of your healthcare provider's directions carefully.
See more dosage directions
Other things to keep in mind about taking LONSURF
- Store LONSURF at room temperature between 68°F and 77°F (20°C to 25°C)
- Don't store LONSURF with other medicines. Keep LONSURF in its own container
- If you store your tablets outside of the original container, any unused LONSURF tablets should be disposed of after 30 days
- Wash your hands after handling LONSURF. Even though it is a pill, it is still chemotherapy
- Make sure your caregiver wears gloves when handling LONSURF
- Note that there is a packet inside the bottle that helps absorb moisture. Do not swallow this material
- Keep LONSURF out of the reach of children
Contact your healthcare provider if:
- You miss a dose. Do not take additional doses to make up for the missed dose. Call your healthcare provider for instructions about what to do for a missed dose
- You have leftover tablets. Your healthcare provider or pharmacist will tell you how to dispose of them properly
Create your treatment calendar
With this simple tool, you can create and print a personalized LONSURF treatment calendar where you can track your doses, temperature, and any side effects you experience. Make sure to share your calendar with your healthcare provider at your next appointment.
Note: If your doctor changes your LONSURF dosage, be sure to create a new treatment calendar.IMPORTANT INFORMATION AND SIDE EFFECTS
Your healthcare provider should check your blood cell counts before you receive LONSURF, at day 15 during treatment, and as needed.
- Low blood counts are common with LONSURF and can sometimes be severe and life-threatening. LONSURF can cause a decrease in your white blood cells, red blood cells, and platelets. Low white blood cells can make you more likely to get serious infections that could lead to death. Your dosage of LONSURF may be reduced or stopped

Tell your healthcare provider right away if you develop any signs of infection such as fever, chills, or body aches.
Almost all patients treated with LONSURF experience side effects at some time. Some common side effects you may experience include:
- Tiredness (fatigue/weakness)
- Nausea
- Vomiting
- Decreased appetite
- Diarrhea
- Abdominal pain
- Fever
Tell your healthcare provider if you have nausea, vomiting, or diarrhea that is severe or that does not go away. These are not all of the possible side effects of LONSURF.
HOW TO MANAGE
SIDE EFFECTS
Your healthcare provider may have ways to help manage some of the side effects of LONSURF tablets. This could include adjusting your treatment plan by delaying or changing your dosage.
The following information may also be helpful to you in managing some of the side effects of LONSURF while under your healthcare provider's care.
This information is not meant to replace your healthcare provider’s advice. Always discuss any side effects with your healthcare provider.
Choose one or more to get helpful ideas:
Tiredness (fatigue/weakness)
- Do the things that are most important first each day. Don’t overdo it
- Take time to rest
- Take naps that are less than 1 hour. Keeping naps short will help you sleep at night
- Try to be active each day. Talk to your healthcare provider about exercise that can help, like going for a 15‑minute walk, doing yoga, or riding an exercise bike
- Make a bedtime routine. Bathing, reading, listening to music, or meditating before you go to bed may help you relax
- Try to sleep at least 8 hours each night
- Ask family members and friends for help with chores, driving to your appointments, shopping, and cooking
- Talk to your healthcare provider. He or she may prescribe medication that can help decrease tiredness
Nausea and vomiting
- A good way to prevent vomiting is to first prevent nausea. It may help to avoid certain foods. Don’t eat greasy, fried, sweet, or spicy foods if you feel sick after eating them
- Eat 5 or 6 small meals a day, instead of 3 big ones (this does not change your dosing schedule)
- Have food and drinks that are warm or cool instead of hot or cold
- Try small bites of popsicles or fruit ices. You can see if sucking on ice cubes helps (stop if the cold temperature bothers you)
- Talk to your healthcare provider, who may prescribe something to help. You can also ask your healthcare provider about acupuncture
Decreased appetite
- Patients with stomach cancer should talk to their healthcare provider for special dietary needs that may be impacted by their condition
- Eat 5 or 6 small meals a day, instead of 3 big ones (this does not change your dosing schedule)
- Drink milkshakes, smoothies, juice, or soup if you do not feel like eating solid foods
- Choose foods that are high in calories and/or protein
- Being active may help you feel hungrier. Talk to your healthcare provider about exercises that can help, like going for a 15-minute walk, stretching, swimming, or riding a bike
- Talk to your healthcare provider, who may suggest that you take extra vitamins or supplements
Diarrhea/abdominal pain
For diarrhea:
- Eat 5 or 6 small meals each day, instead of 3 big ones (this does not change your dosing schedule)
- Ask your healthcare provider about foods high in sodium and potassium. Because your body can lose these minerals when you have diarrhea, it is important to replace them. Foods that are high in sodium and potassium include bananas, oranges, peach and apricot nectar, and boiled or mashed potatoes
- Eat low‑fiber foods
- Drink 8 to 12 cups of clear liquids each day
- Drink liquids at room temperature slowly
- Talk with your healthcare provider, who may prescribe medicine to help. Do not take any medicine without discussing it beforehand
- Try deep breathing, yoga, or other ways to relax. This can help with muscle tension, anxiety, and pain
For abdominal pain:
- Exercise regularly
- Eat plenty of foods that are high in fiber such as fruits and vegetables
- Avoid foods that produce gas
- Let your caregiver know about your pain so he or she can try and help
Fever
- Drink plenty of liquids, like water, juice, and broth because a fever can cause fluid loss and dehydration
- Rest
- Keep cool by dressing in light clothing and sleeping with only a sheet
- Call your healthcare provider immediately if you have a fever or other signs of an infection. You can use the thermometer in the Starter Kit to check your temperature each day
You can call the Taiho Oncology 24/7 hotline with questions about side effects with LONSURF at 1‑844‑US‑TAIHO (1‑844‑878‑2446). You may also report side effects to the FDA at 1‑800‑FDA‑1088.
SEE ALL INDICATIONS
INDICATIONS
LONSURF is a prescription medicine used:
- alone or in combination with the medicine bevacizumab to treat adults with colorectal cancer:
- that has spread to other parts of the body, and
- who have been previously treated with certain chemotherapy medicines
- alone to treat adults with a kind of stomach cancer called gastric cancer including adenocarcinoma of the gastroesophageal junction:
- that has spread to other parts of the body, and
- who have been previously treated with at least 2 types of treatment which included certain medicines
It is not known if LONSURF is safe and effective in children.
INDICATIONS
LONSURF is a prescription medicine used:
- alone or in combination with the medicine bevacizumab to treat adults with colorectal cancer:
- that has spread to other parts of the body, and
- who have been previously treated with certain chemotherapy medicines
- alone to treat adults with a kind of stomach cancer called gastric cancer including adenocarcinoma of the gastroesophageal junction:
- that has spread to other parts of the body, and
- who have been previously treated with at least 2 types of treatment which included certain medicines
It is not known if LONSURF is safe and effective in children.
IMPORTANT SAFETY INFORMATION
LONSURF may cause serious side effects, including:
- Low blood counts. Low blood counts are common with LONSURF and can sometimes be severe and life-threatening. LONSURF can cause a decrease in your white blood cells, red blood cells, and platelets. Low white blood cells can make you more likely to get serious infections that could lead to death. Your healthcare provider should do blood tests before you receive LONSURF, at day 15 during treatment with LONSURF, and as needed to check your blood cell counts. Your healthcare provider may lower your dose of LONSURF or stop LONSURF if you have low white blood cell or platelet counts
Tell your healthcare provider right away if you get any of the following signs and symptoms of infection during treatment with LONSURF: fever, chills, or body aches.
Before taking LONSURF, tell your healthcare provider about all of your medical conditions, including if you:
- Have kidney or liver problems
- Are pregnant or plan to become pregnant. LONSURF can harm your unborn baby
- Females who can become pregnant: Your healthcare provider will do a pregnancy test before you start treatment with LONSURF. You should use effective birth control during and 6 months after the last dose of treatment with LONSURF. Tell your healthcare provider immediately if you become pregnant
- Males, while on treatment and for 3 months after your last dose of LONSURF, you should use a condom during sex with female partners who are able to become pregnant. Tell your healthcare provider right away if your partner becomes pregnant while you are taking LONSURF
- Are breastfeeding or plan to breastfeed. It is not known if LONSURF passes into your breast milk. Do not breastfeed during treatment with LONSURF and for 1 day after your last dose of LONSURF
Tell your healthcare provider about all the prescription and over-the-counter medicines, vitamins, and herbal supplements you take.
The most common side effects of LONSURF when used alone include low blood counts, tiredness and weakness, nausea, decreased appetite, diarrhea, vomiting, stomach-area (abdominal) pain, and fever.
The most common side effects of LONSURF when used in combination with bevacizumab include low blood counts, tiredness and weakness, nausea, certain abnormal liver function blood tests, decreased salt (sodium) in your blood, diarrhea, stomach-area (abdominal) pain, and decreased appetite.
Tell your healthcare provider if you have nausea, vomiting, or diarrhea that is severe or that does not go away.
These are not all of the possible side effects of LONSURF. For more information, ask your healthcare provider. Call your doctor for medical advice about side effects.